CASE OF THE WEEK
A female patient in her late 60s underwent surgical removal of bladder tumor. The first pathology report had the diagnosis of poorly differentiated carcinoma.
Contributors :
Vinicius Barros Figueiredo
Oncoclinicas Precision Medicine
Belo Horizonte, Minas Gerais, Brazil
Daniel Athanazio
Oncoclinicas Precision Medicine
Federal University of Bahia
Salvador, Bahia, Brazil
What is the correct diagnosis?
Neuroendocrine carcinoma
Urothelial carcinoma, nested subtype
Paraganglioma
Nephrogenic adenoma
Urothelial carcinoma, NOS
Paraganglioma
Paraganglioma
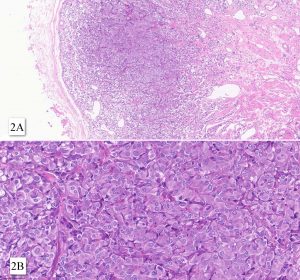
Besides GATA3 and chromogranin A expression (see figures), tumor cells were also positive for synaptophysin, S100 protein and INSM1. SDHB expression was retained. Tumor cells did not express pan-keratins, p40, p63, PAX8, CD34 and smooth muscle actin.
Paraganglioma accounts less than 1% of all bladder neoplasms and less than 10% of paragangliomas are found in the urinary bladder. Symptoms may include headache, paresthesia, dyspnea, angina, hematuria, and lower urinary tract symptoms. The vast majority of pediatric cases and about half of the adult cases are associated with germline mutations, most frequently in the SDHB gene.
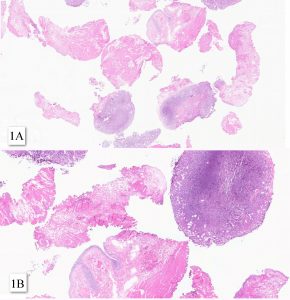
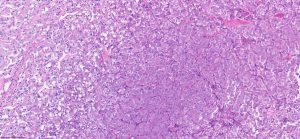
Paragangliomas of the bladder may have an epicenter in bladder muscularis propria, or in intact or ulcerated mucosa. At microscopy, the tumor shows a nested growth pattern with a Zellballen appearance. Nests are delineated by a delicate fibrovascular network and sustentacular cells. Tumor cells are round to oval may show pleomorphism or hyperchromasia. The cytoplasm may be eosinophilic or mirror the amphophilic to basophilic appearance of pheochromocytomas. Paragangliomas of the bladder usually involves muscularis propria and express GATA3 – two features that may lead to a misdiagnosis of advanced urothelial carcinoma.
Although rare, bladder paraganglioma should be considered in the differential diagnosis of bladder neoplasm with nested pattern of growth. An expanded panel of immunostain can easily distinguish urothelial carcinoma (keratin positive) from paragangliomas (keratin negative; positive for neuroendocrine markers).
Risk stratification of paragangliomas is challenging and metastasis may develop many after surgical treatment. Grading scores systems used for pheochromocytomas may be used, with variable performance on prognostic prediction. Aggressive neoplasms are associated with germline SDHB mutations and somatic SETD2 or ATRX mutations, MAML3 fusions, WNT-altered pathway and TERT activation. In a recent cohort of 27 paragangliomas of the bladder, three developed recurrence and one patient died of metastatic disease within one year after surgery.
1. de Krijger RR, Gill AJ, Mete O, Merino MJ, Cheng L, Varma M. Paraganglioma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours. Lyon (France): International Agency for Research on Cancer; 2022. . (WHO classification of tumours series, 5th ed.; vol. 8). https://publications.iarc.fr/610.
2. Zhao Y, Zhang Z, Wang S, Wen J, Wang D, Ji Z, Zhang Y, Li H. A retrospective study of paraganglioma of the urinary bladder and literature review. Front Surg. 2024 Apr 5;11:1348737
3. Beilan JA, Lawton A, Hajdenberg J, Rosser CJ. Pheochromocytoma of the urinary bladder: a systematic review of the contemporary literature. BMC Urol. 2013 Apr 29;13:22.
4. Iwamoto G, Kawahara T, Tanabe M, Ninomiya S, Takamoto D, Mochizuki T, et al. Paraganglioma in the bladder: a case report. J Med Case Rep. (2017) 11:306. 10.1186/s13256-017-1473-2
Vinicius Barros Figueiredo
Oncoclinicas Precision Medicine
Belo Horizonte, Minas Gerais, Brazil
Daniel Athanazio
Oncoclinicas Precision Medicine
Federal University of Bahia
Salvador, Bahia, Brazil
Urinary bladder
Bladder; Paranganglioma; Bladder Neoplasms.