CASE OF THE MONTH
47-year-old man with penile lesion
Contributors :
Daria Afromeeva
Kyle James Lockhart
Levent Trabzonlu, email: ltrabzo@uic.edu
Institution: Department of Pathology, University of Illinois at Chicago, Chicago, IL
What is the diagnosis?
Spindle cell hemangioma
Spindle cell melanoma
Dermatofibroma
Kaposi sarcoma
Sarcomatoid squamous cell carcinoma
What is the best immunohistochemical marker to distinguish this entity from other vascular neoplasms?
ERG
CD31
CD34
FLI-1
HHV-8
Q1- Kaposi sarcoma
Q2- HHV-8
Kaposi sarcoma
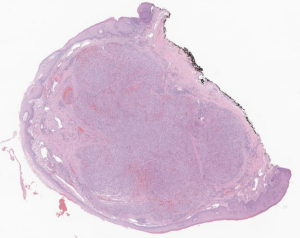
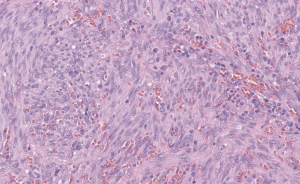
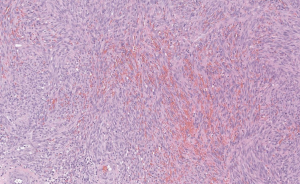
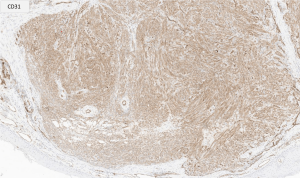
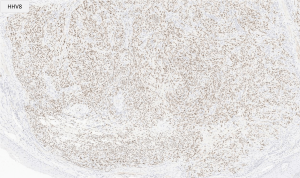
We presented a rare case of primary penile Kaposi sarcoma. The patient was a 47-year-old man with a past medical history of HIV on a daily regimen of highly active antiretroviral therapy (HAART). The lesion was described as a bump that occasionally bleeds and was painful. The patient denied penile discharge, blistering, fever, chills, weight loss, or night sweats. At the time of diagnosis, the HIV viral load was undetectable, and the CD4-positive T-cell count was reported as >800/mm3 two weeks prior. The sections of the excision biopsy showed a well-circumscribed, dermal-based lesion composed of monomorphic, low-grade spindle cells creating slit-like spaces with extravasated red blood cells. Immunohistochemical stains showed that the spindle cells are diffusely positive for CD31 and HHV-8, confirming the diagnosis of Kaposi sarcoma.
Kaposi sarcoma is a slow-growing angioproliferative tumor typically occurring in patients with immunosuppression, including those with acquired immunodeficiency syndrome (AIDS) or undergoing chronic immunosuppressive treatment related to previous organ transplants. In HIV-positive patients, Kaposi sarcoma is an AIDS-defining illness and indicates the progression of HIV to AIDS. This designation supersedes the requirement of having a low CD4-positive T-cell count. Patients with Kaposi sarcoma classically have a low CD4-positive T-cell count and a high HIV viral load. However, recent publications demonstrated that the disease can still occur in patients with normal CD4-positive T-cell counts and low or undetectable viral loads, as seen in the case presented here.
A literature review with key terms focusing on “Kaposi sarcoma”, “penis/penile”, and “genitalia” in HIV-positive patients shows a limited number of reports. Most cases occurred in patients with advanced disease-related immunosuppression and presented with widespread cutaneous lesions with further progression of secondary lesions on the penis. The prevalence of genital lesions as a progression of the disease has been estimated to account for 20% of those diagnosed with Kaposi sarcoma, with only 3% presenting with a primary lesion in this area. Notably, there has been one other case published by Lebari et al. in 2014 describing a primary penile lesion despite HAART with undetectable viral load and an adequate CD4-positive T-cell count.
The differential diagnosis of Kaposi sarcoma depends on the location of the lesion, as it can mimic a wide variety of spindle cell neoplasms. In the penis, the differential diagnosis includes spindle cell melanoma, dermatofibroma, and other vascular tumors, including angiosarcoma. In the presence of classic morphology, a simple immunohistochemical panel to include HHV8 would be enough to render the diagnosis, like the case presented here. More challenging cases might result in a more comprehensive work-up; however, the most important determinator for reaching the diagnosis would be to keep this rare entity in mind.
Although primary penile Kaposi sarcoma is a rare entity, it is important to recognize that it should be considered in a patient with history of HIV, even in the presence of a normal CD4-positive T-cell count and an undetectable HIV viral load.
1. Farshidpour M, Marjani M, Baghaei P, Tabarsi P, Masjedi H, Asadi Kani ZF, Nadji SA, Mansouri D. Disseminated Kaposi’s Sarcoma with the Involvement of Penis in the Setting of HIV Infection. Indian J Dermatol. 2015 Jan-Feb;60(1):104.
2. Klein LT, Lowe FC. Penile gangrene associated with extensive Kaposi’s sarcoma in patients with the acquired immunodeficiency syndrome. Urology 1995;46:425-427
3. Lowe FC, Lattimer DG, Metroka CE. Kaposi’s sarcoma of the penis in patients with acquired immunodeficiency syndrome. J Urol. 1989 Dec;142(6):1475-7.
4. Tammam A, Abdulrahman A, Ebrahim M, Mohammad B, Kanan A, Nada S, Abdulrahman A, Ahmad A. Penile Kaposi Sarcoma as an initial manifestation of HIV infection: A case report and literature review. IDCases. 2022 Jul 19;29:e01576
5. Rosen, T., Hoffman, J. and Jones, A. (1999), Penile Kaposi’s sarcoma. Journal of the European Academy of Dermatology and Venereology, 13: 71-73.
6. Angulo JC, Lopez JI,Unda-Urzaiz M, et al. Kaposi’s sarcoma of the penis as an initial manifestation of AIDS. A report of two cases. Urol Int 1991;46:235-237.
7. Lebari D, Gohil J, Patnaik L, Wasef W. Isolated penile Kaposi’s sarcoma in a HIV-positive patient stable on treatment for three years. International Journal of STD & AIDS. 2014;25(8):607-610.
Daria Afromeeva
Kyle James Lockhart
Levent Trabzonlu, email: ltrabzo@uic.edu
Institution: Department of Pathology, University of Illinois at Chicago, Chicago, IL
Penis
Penis, kaposi sarcoma, primary, HIV